Type 1 diabetes: A new starting point to delay autoimmune response

Regulatory T cells (Tregs) prevent excessive immune reactions in healthy people. In the development of autoimmune type 1 diabetes, this protection is not sufficiently effective. Researchers at Helmholtz Zentrum München and LMU Munich have now deciphered a mechanism that impairs Treg differentiation and stability.
In the study, when researchers inhibited the molecule that triggers this mechanism, an increased number of functional Tregs were formed again and autoimmune activation was reduced. This may represent a new molecular target to delay or even prevent the development of type 1 diabetes. The study was carried out within the framework of the German Center for Diabetes Research (DZD), and the results have now been published in Nature Communications.
Type 1 diabetes is the most common metabolic disease in children and adolescents. In this autoimmune disease, the body’s own immune cells gradually destroy the insulin-producing beta cells in the pancreas. Normally, Tregs prevent an attack on the body’s own cells. However, during the development of type 1 diabetes, this protection is insufficient. The team led by Professor Carolin Daniel is investigating why this is the case. She is research group leader at the Institute of Diabetes Research (IDF) at Helmholtz Zentrum München, scientist in the DZD and professor for immune modulation at Ludwig- Maximilians-Universität in Munich. The researchers have now deciphered a molecular mechanism that, during an early phase of type 1 diabetes, leads to the formation of decreased numbers of functional Tregs.
Elevated levels of miRNA142-3p contribute to the development and progression of autoimmunity
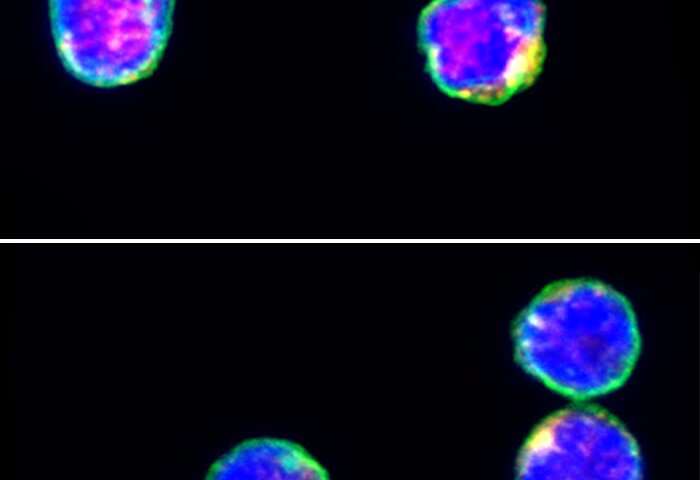
The microRNA miRNA142-3p plays a decisive role in this process. MicroRNAs can suppress the expression of individual genes. “During the development of autoimmunity in type 1 diabetes, we were able to detect an increased abundance of miRNA142-3p. This leads to a reduced expression of the protein Tet2 in T-helper cells,” said first author Martin Scherm. As a consequence, faulty epigenetic changes occur in the Foxp3 gene of the regulatory T cells. A decreased number of these important immune cells are formed, and the Tregs are no longer as stable. “Our research results show a direct link between miRNA142-3p and the impaired function of regulatory T cells, which subsequently contributes to the development and progression of autoimmunity,” said senior author Carolin Daniel, summarizing the results of this study.
New target for future intervention strategies
In order to investigate whether the findings could also open up new therapeutic approaches in the future, the scientists specifically blocked the miRNA142-3p molecule. This improved the formation and stability of the regulatory T cells. In the animal model, the autoimmune response to the insulin-producing beta cells also decreased.
“The detailed investigation of the underlying mechanisms led to the identification of promising targets for future intervention strategies. The targeted inhibition of miRNA142-3p could open up new ways to reduce the activity of the immune system against its own insulin-producing cells,” said Professor Anette Ziegler, head of the IDF.
Source: Read Full Article