Generating Megakaryocytes and Platelets from Adipocytes

Adipocytes can be converted into mesenchymal stem cells, which can then be converted into megakaryocytes. These megakaryocytes can be used to produce platelets, which may be a source of safer platelet transfusions.
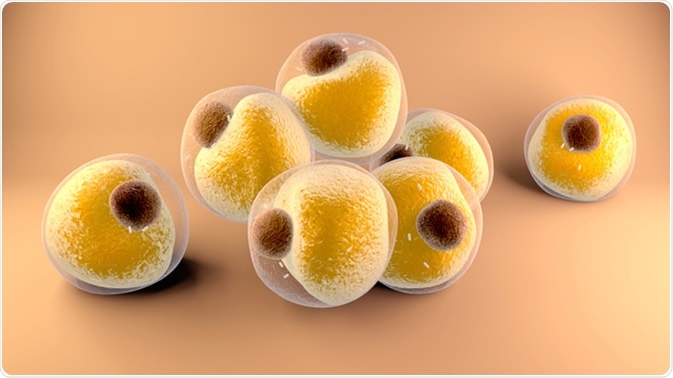
What are adipocytes?
Adipocytes are specialized cells that store energy as fat, they are mainly comprised of adipose tissues. Adipocytes differentiate from mesenchymal stem cells; thus, they are part of the mesodermal lineage.
There are two adipose tissue types: white adipose tissue (WAT; also known as white fat) and brown adipose tissue (BAT; also known as brown fat). WAT contains a large lipid complex surrounded by cytoplasm, the lipid complex is mainly comprised of triglycerides and cholesteryl esters in a semi-liquid state. BAT cells contain multiple smaller lipid complexes surrounded by a large cytoplasm, also they contain a large number of mitochondria.
Megakaryocytes and platelets
Platelets (also known as thrombocytes) are a crucial to blood clot formation. Defects with platelet regulation can lead to various different disorders and diseases such as thrombocytopenia.
Thrombocytopenia is characterized by an abnormally low level of thrombocytes in the blood, which can be caused by malignancy, chemotherapy, autoimmune disorders, infections, and inherited platelet disorders. Platelet transfusions can be used to treat thrombocytopenia as well as other platelet disorders, however, they are not completely safe, and rejections can occur.
The development of platelets starts with mesenchymal stem cells (MSCs). These MSCs differentiate into immature megakaryocytes (MKs), which then further differentiate into mature MKs with unique functions. Mature MKs release platelets into the blood.
One possible method to reduce the negative effects of platelet transfusions is to derive platelets from stem cells taken from the host, so rejection is not an issue. Platelets have been artificially created from numerous sources including hematopoietic stem cells (HSCs), embryonic stem cells (ESCs), and induced pluripotent stem cells (iPSCs).
Generating megakaryocytes and platelets from adipocytes
Adipose-derived stromal cells (ASCs) can be an effective source of platelets, as they don’t require any gene transfer; thus, differentiation is straightforward. This is because they already contain many important genes known for MK differentiation and platelet production. HSCs and iPSCs require recombinant thrombopoietin (rTPO) to differentiate into MKs, but ASCs do not, which is what makes them a more advantageous choice when trying to produce platelets. Although ASCs are promising, they contain heterogenous cells which makes them not completely viable as a donor-independent source of platelets.
Adipose-derived mesenchymal stem cells (ASCLs) can also be used to produce platelets. It has been shown that ASCLs that are cultured in MK lineage induction (MKLI) media will develop similar characteristics to cord-blood-derived MKs (expression of MK specific cell surface markers, CD41 and CD42b).
Tests were performed on ASCL-derived platelets (ASCL-PLTs) to ensure that they express the right cell surface markers and intracellular proteins to be used in transfusions. These tests showed that ASCL-PLTs express cell adhesion markers, which is important for the function of platelets.
Functional analysis of adipose-derived mesenchymal stem cell-derived platelets
Platelets are involved in hemostasis and their regulation is crucial for wound healing and the formation of blood clots. Platelets are activated by external stimulation, such as contact with exposed subendothelial cells. ASCL-PLTs and platelet concentrates were compared and it was discovered that ASCL-PLTs reacted to thrombin, adrenaline, calcium, and magnesium in a similar fashion to platelet concentrates. ASCL-PLTs also have a higher surface exposure of P-selectin (a marker for platelet activation) than on platelet concentrates.
Conclusion
MKs and platelets can be produced from many different cell progenitors. The production of platelets from ASCLs is promising because transfusion of these cells may be associated with lower risks than donor platelets.
Sources
- http://www.bloodjournal.org/content/bloodjournal/133/7/633.full.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3730538/
Further Reading
- All Hematology Content
- What is Hematology?
- What is Hematopoiesis?
- Hematology Tests
- Hematology Treatments
Last Updated: Mar 28, 2019
Written by
Samuel Mckenzie
Sam graduated from the University of Manchester with a B.Sc. (Hons) in Biomedical Sciences. He has experience in a wide range of life science topics, including; Biochemistry, Molecular Biology, Anatomy and Physiology, Developmental Biology, Cell Biology, Immunology, Neurology and Genetics.
Source: Read Full Article