Potential new cancer treatment a step closer

QIMR Berghofer researchers have discovered a potential new cancer immunotherapy target that involves switching off a regulatory cell to stop tumors growing and spreading.
The study findings have been published today in Cancer Discovery, a journal of the American Association for Cancer Research.
Senior researcher and head of QIMR Berghofer’s Cancer Immunoregulation and Immunotherapy Laboratory, Associate Professor Michele Teng, said in future the discovery could potentially help treat patients with cancers where other current immunotherapies have not worked.
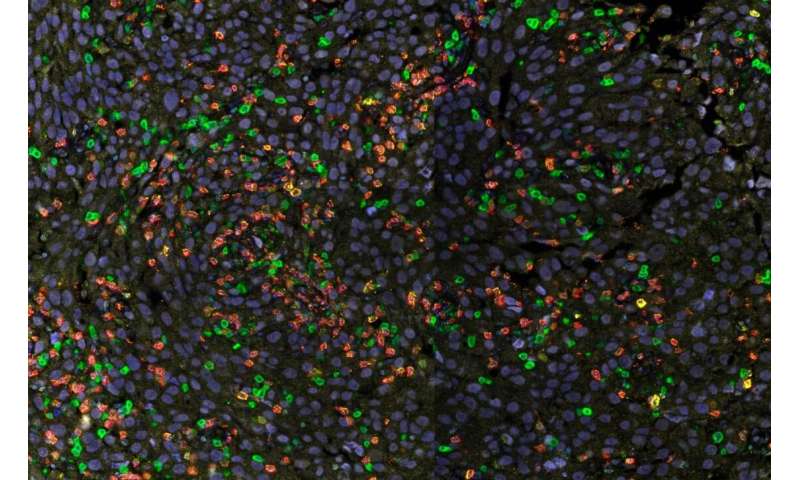
“Our work on mice shows for the first time that many tumors display the molecule MR1 on their cell surface, and when it’s present, this molecule turns on an important regulatory cell that prevents the body’s own immune system from fighting the cancer,” Associate Professor Teng said.
“We found if a type of regulatory cell called MAIT (mucosal-associated invariant T) cells are turned on, they stop immune or white blood cells known as T and NK cells from attacking and killing off tumor cells.
“The cancer is effectively creating its own defense mechanism to evade immune attack and survive. The display of MR1 activates the MAIT cells, which in turn switch off cancer-fighting T and NK cells.
“While other regulatory cells of the immune system are known to stop T and NK cells from killing tumor cells, this is the first time it’s been shown that these regulatory MAIT cells can do this job.”
Associate Professor Teng said her team found that by giving mice an antibody that blocked MR1, this stopped the MAIT cells from becoming activated, and the T and NK cells could respond, slowing cancer growth and stopping it spreading.
“This work demonstrates that antibodies that block MR1 could in future be an effective new immunotherapy,” Associate Professor Teng said.
“It probably won’t work on every cancer, but it looks like it could be effective in treating cancers that can display the MR1 molecule. It also means this display of MR1 could be used to screen which patients would respond to this immunotherapy.
“We now need to replicate this research in humans.”
Associate Professor Teng said while the research was at a very early stage and required more work, it was promising.
“The next step is to try to understand what kind of human tumors display MR1 as a protective mechanism, which would then help us identify which tumors would respond best to MR1-blocking immunotherapy,” she said.
“Immunotherapies have been effectively used to treat more than 15 different cancer types but the proportion of patients that respond for each cancer can differ.
Source: Read Full Article