Bronchiectasis Symptoms and Diagnosis

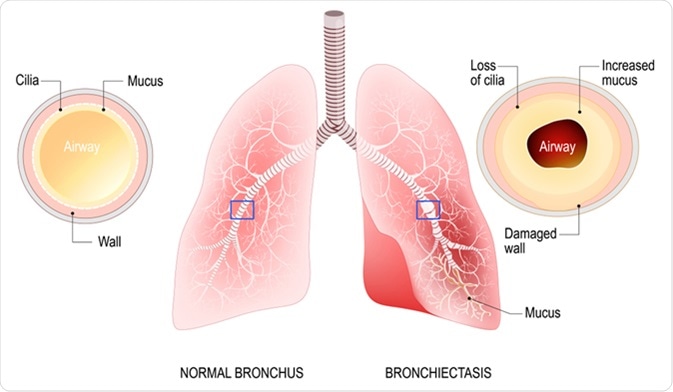
Bronchiectasis is a chronic condition of the respiratory system that is due to abnormal widening of the airways as a consequence of an initial damaging factor. The bronchi, located between the trachea and the alveoli of the lungs, produce a small amount of mucus in physiological conditions, which aids in removing pathogenic particles, and ensures that the airways remain clean and moist.
In bronchiectasis, the bronchi become permanently dilated and their ability to clear out excessive amounts of mucus is impaired. This leads to an excessive buildup of mucus, which promotes the growth of pathogenic microorganisms that cause recurring infections and lasting damage to the airways.
There are a number of primary causes of bronchiectasis, including both acquired and congenital conditions. A large number of cases of bronchiectasis are classified as idiopathic, with no obvious underlying cause. Bronchiectasis can occur at any age, although it is more commonly acquired later in life, and it affects more women than men. Moreover, while it is still classified as a rare disease, it is growing in prevalence worldwide.
What are the symptoms of bronchiectasis?
The main symptoms of bronchiectasis include a chronic cough, excessive sputum production, and recurrent infections of the respiratory system due to the buildup of mucus in the airways. Patients will experience a persistent cough that brings up phlegm and may bring up blood in the case where there is significant damage to the bronchi. The severity of symptoms will vary depending on an individual, as well as the underlying cause of the disease, and will typically get worse if there is an infection of the lungs. Bronchiectasis may affect a few parts of the lung or be limited to a single lobe, depending on the etiology of the disease.
Other symptoms may include shortness of breath, chest pain, and joint pain. Clubbing of the fingernails may also occur, where the skin underneath the nail becomes thick and the fingernails become enlarged and bulbous.
As the disease progresses, symptoms tend to become more regular and severe. Since suppression of the infection and clearing of secretions become more difficult, the goal of therapy is to minimize symptoms, prevent further loss of lung function, and ensure the best possible quality of life.
How is bronchiectasis diagnosed?
Diagnostic testing for bronchiectasis will largely depend on the etiology of the disease. Since there is a great number of causes for bronchiectasis, it is not possible to routinely test each patient for all possible underlying conditions. As such, it is important for the clinician to recognize the most probable patient phenotypes, and use deferential testing for disorders, such as cystic fibrosis (CF), primary ciliary dyskinesia (PCD) or non-tuberculous mycobacterial infections.
Diagnosing the underlying condition responsible for causing the bronchiectasis is key in determining the right treatment, and will greatly improve patient’s outcome. The European Respiratory Society guidelines for bronchiectasis recommend a minimal set of tests for diagnosing the cause of bronchiectasis. Additional tests may be ordered in specific clinical settings or in patients with a disease that is severe or progresses rapidly.
After medical screening and an initial diagnosis of bronchiectasis, a physician will order diagnostic tests consisting of a complete blood count, as well as immunoglobulins that test for allergic bronchopulmonary aspergillosis. Further specific testing may be necessary to identify the underlying cause.
High resolution computer tomography (HRCT) is recommended for giving the right differential diagnosis of bronchiectasis. For example, since the features of a regular computer tomography (CT) scan of post-tuberculous bronchiectasis differ from those seen in patients with non-tuberculous mycobacteria (NTM) related disease, HRCT provides an additional aid in differential diagnosis. Prior identification of dilation of the airways is a prerequisite for running an HRCT scan.
Sources
- NHS: Bronchiectasis https://www.nhs.uk/conditions/bronchiectasis/
- British Lung Foundation: Bronchiectasis https://www.blf.org.uk/support-for-you/bronchiectasis/what-is-it
- American Thoracic Society, Patient Education Information Series, Bronchiestasis www.thoracic.org/…/chapter-4-bronchiectasis.pdf
- JD Chalmers, SH Chotirmall, Bronchiectasis: new therapies and new perspectives, The Lancet Respiratory Medicine, 2018, https://doi.org/10.1016/S2213-2600(18)30053-5
- Contarini M, Finch S, Chalmers JD. Bronchiectasis: a case-based approach to investigation and management. Eur Respir Rev 2018; 27:180016, https://doi.org/10.1183/16000617.0016-2018
Further Reading
- All Bronchiectasis Content
- Bronchiectasis Treatment
- Bronchiectasis Complications
- What Causes Bronchiectasis?
- What is Bronchiectasis?
Last Updated: Jan 15, 2019
Source: Read Full Article